Ever feel that peculiar tickle at the back of your throat? Or perhaps you've glanced in the mirror and noticed something unusual with that little punching bag-like appendage dangling down? We're talking about your uvula, a small but mighty player in your overall health. While often overlooked, this fleshy extension at the back of your throat is critical for everything from clear speech and smooth swallowing to immune defense. When things go wrong with it, life can get uncomfortable quickly.
Understanding uvula pathologies—and how cutting-edge tools like AI are now enhancing their diagnosis—is essential for timely and effective treatment. You don't have to be a medical expert to recognize the signs your body is sending. This guide will walk you through what to look for, how diagnoses are made, and how technology is stepping in to make the process more accurate and efficient than ever before.
At a Glance: Your Uvula Health Checklist
- Crucial Role: Your uvula aids speech, swallowing, immune response, and saliva production.
- Warning Signs: Persistent sore throat, difficulty swallowing, choking, snoring, or a visible change in your uvula's appearance warrant a doctor's visit.
- Common Issues: Swelling (uvulitis), elongation, bifurcation, and lesions are among the frequent problems.
- Traditional Diagnosis: Involves medical history, physical exam, and diagnostic tests like throat swabs or imaging.
- AI's Advantage: Artificial intelligence is emerging as a powerful tool to accelerate accurate detection through image analysis and symptom pattern recognition.
- Prevention: Hydration, avoiding irritants, and managing reflux can help prevent some uvula issues.
- Next Steps: If symptoms persist, don't delay—consult your doctor.
The Unsung Hero: Why Your Uvula Matters More Than You Think
That small, fleshy pendant hanging at the soft palate's edge is your uvula, a surprisingly active part of your anatomy. Far from just a decorative piece, it plays several vital roles in your daily functions and overall well-being. Think of it as a multi-talented assistant orchestrating harmony in your throat.
It helps with speech articulation, particularly in forming sounds for specific languages. It's also crucial for swallowing, working to block the nasal cavity and prevent food or liquid from entering your nose. Beyond these mechanics, the uvula contributes to your immune response and even aids in saliva production, keeping your throat moist and healthy. When any of these functions are compromised by an abnormality, you quickly notice the impact on your comfort and quality of life.
When Your Uvula Signals Trouble: Common Symptoms to Watch For
Your body has a sophisticated alarm system, and your uvula is no exception. Abnormalities often manifest through a range of symptoms that, while sometimes subtle, can significantly disrupt your daily routine. Recognizing these signals early is key to seeking prompt medical attention and getting back to feeling your best.
You should consult a doctor if you experience persistent symptoms that don't resolve on their own. These might include a nagging sore throat, difficulty swallowing your food, a feeling of choking, new or worsened snoring, or any noticeable change in your uvula's appearance.
More Than Just a Sore Throat: The Spectrum of Uvular Discomfort
Symptoms of uvula abnormalities can vary widely, but they often point to an underlying issue. Here's a comprehensive list of what to look out for:
- Visible Changes: Noticeable alteration in the uvula's shape, size, or color. It might appear swollen, elongated, or unusually red.
- Persistent Irritation: A continuous sore throat or an irritating sensation at the back of the throat that doesn't go away.
- "Stuck" Sensation: Feeling like there's something lodged in your throat, even when you haven't eaten recently.
- Swallowing Difficulties (Dysphagia): Pain or effort required to swallow, or a sensation of food getting caught.
- Frequent Choking or Gagging: An increased tendency to choke on food or liquid, or an exaggerated gag reflex.
- Sleep Disturbances: New or increased snoring, or symptoms indicative of sleep apnea, which can occur if an enlarged uvula obstructs the airway during sleep.
- Saliva Issues: Either excessive salivation (hypersalivation) or a feeling of dry mouth, both of which can be linked to uvular problems.
- Bad Breath (Halitosis): Often a sign of infection, especially if accompanied by other throat symptoms.
- Unusual Growths: Visible bumps, ulcers, white patches, or discoloration on the uvula itself.
If any of these symptoms persist beyond a few days or seem to be worsening, it's wise to schedule an appointment with your doctor. Early intervention can prevent minor issues from becoming more complex.
Decoding Uvular Woes: A Deep Dive into Pathologies
Uvula abnormalities aren't always serious, but they're rarely comfortable. Understanding the common types of uvula pathologies can help you grasp what might be happening and why. They often fall into categories of inflammation, structural anomalies, or growths, each with distinct characteristics and potential implications.
Uvulitis: The Swollen Uvula
Perhaps the most common uvula pathology, uvulitis refers to inflammation and swelling of the uvula. It often accompanies general throat infections, such as strep throat, or can be triggered by allergies, dehydration, or irritants like smoking. When your uvula swells, it can feel like a lump in your throat, causing discomfort, difficulty swallowing, and even gagging. Identifying and treating the underlying cause, often an infection, is critical to resolve uvulitis. For insights into what to look for if you suspect strep throat, further reading can be helpful.
Elongated Uvula
Sometimes, the uvula is simply longer than average. While this can be a harmless anatomical variation, an overly elongated uvula can become problematic. It can brush against the back of the tongue or throat, triggering a persistent cough, gag reflex, or a feeling of something being stuck. Critically, an elongated uvula can contribute to snoring and obstructive sleep apnea by partially blocking the airway during sleep, making it harder to breathe properly.
Bifid Uvula: The Split Uvula
A bifid uvula is a congenital anomaly where the uvula appears partially split or notched, resembling a snake's tongue. Often discovered incidentally during a routine examination, a bifid uvula is usually benign and causes no symptoms. However, in rare cases, it can be a subtle indicator of a more significant underlying condition, such as a submucous cleft palate, which might affect speech or swallowing in children. Most often, no treatment is needed unless functional problems arise.
Lesions & Growths: From Cysts to Tumors
The uvula, like any other tissue, can develop various lesions or growths. These can range from benign conditions to more concerning issues:
- Cysts: Small, fluid-filled sacs that are typically harmless and often resolve on their own.
- Papillomas: Benign, wart-like growths often caused by the Human Papillomavirus (HPV).
- Ulcers: Open sores that can result from trauma, infection, or other systemic conditions.
- Tumors: While rare, malignant tumors can develop on the uvula, necessitating immediate medical evaluation and biopsy.
Any persistent bump, ulcer, or growth on your uvula should be examined by a doctor to rule out serious conditions.
Trauma and Irritant Exposure
The uvula can also suffer trauma from enthusiastic coughing, vomiting, or even medical procedures. Burns from hot food or drinks are also possible. Additionally, consistent exposure to irritants like cigarette smoke, alcohol, or even chronic acid reflux can irritate and inflame the uvula over time. For effective strategies for managing chronic acid reflux, exploring treatment options is key to preventing long-term damage.
The Diagnostic Journey: How Doctors Pinpoint the Problem
When you present with uvula-related symptoms, your doctor embarks on a systematic diagnostic journey. This process combines your personal health narrative with physical observations and, when necessary, advanced testing. The goal is always to accurately identify the cause of your discomfort, paving the way for targeted and effective treatment.
Step 1: Comprehensive Medical Evaluation
Your journey begins with a conversation. Your doctor will take a detailed medical history, asking about:
- Symptom Duration and Severity: When did symptoms start? How have they progressed?
- Recent Illnesses: Have you had a cold, flu, or other infections lately?
- Allergies: Do you have known allergies, environmental or food-related, that might be triggering a reaction?
- Lifestyle Factors: Smoking history, alcohol consumption, exposure to environmental irritants.
- Medical Conditions: History of acid reflux (GERD), previous throat surgeries, or any family history of congenital anomalies.
This conversation helps build a comprehensive picture, often providing crucial clues to the underlying problem.
Step 2: Physical Examination and Visual Inspection
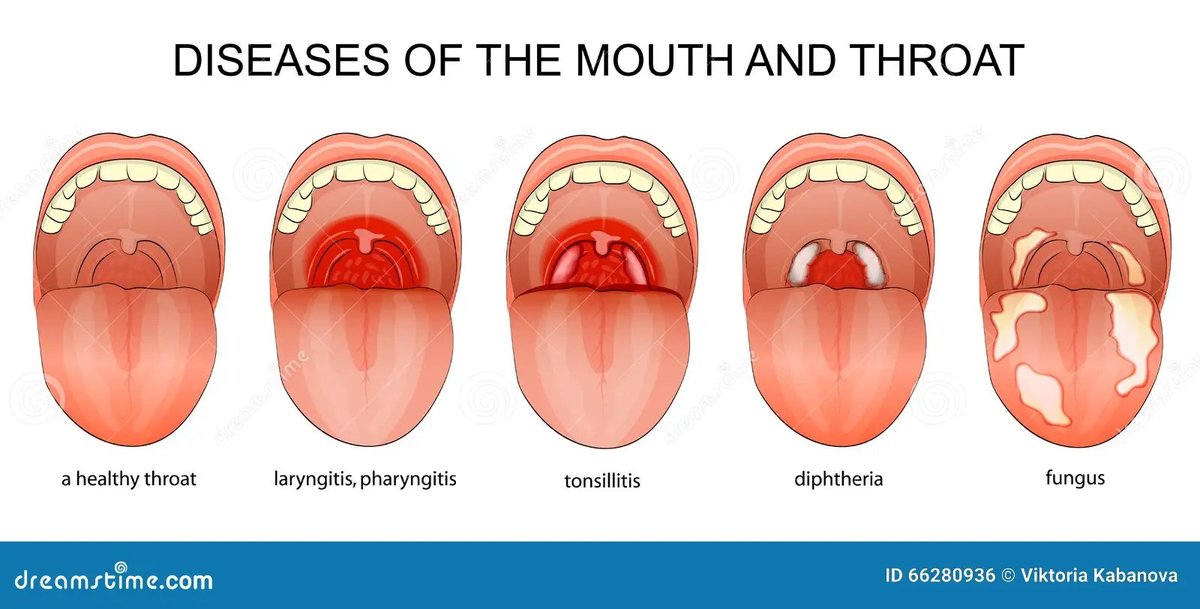
Next, your doctor will perform a thorough physical examination. Using a bright light source and a tongue depressor, they will visually inspect your uvula and the surrounding tissues of your throat and mouth. They'll look for:
- Color Changes: Redness (indicating inflammation or infection), white patches (possibly fungal infections), or other discolorations.
- Size and Shape: Swelling (uvulitis), elongation, or a bifid (split) appearance.
- Presence of Growths: Cysts, papillomas, ulcers, or any suspicious masses.
- Signs of Trauma: Scratches, tears, or burns.
For a more detailed view, especially if the initial inspection is unclear, a flexible fiberoptic nasopharyngoscope might be used. This thin, flexible tube with a camera provides a magnified, illuminated view of the entire throat, including areas not easily visible otherwise. To learn more about flexible fiberoptic nasopharyngoscopy, it's a minimally invasive procedure that offers significant diagnostic benefits.
Step 3: Advanced Diagnostic Tests and Imaging
Depending on the initial findings, your doctor may recommend further tests to confirm a diagnosis or rule out other conditions:
- Throat Swab and Laboratory Tests: If an infection is suspected (like bacterial or streptococcal pharyngitis), a throat swab will be taken for a culture or rapid antigen test. Blood tests may also be ordered to check for systemic infection or widespread inflammation markers.
- Allergy Testing: If allergies are believed to be contributing to uvula swelling, your doctor might suggest skin prick tests or blood IgE level tests to pinpoint specific allergens. For more on identifying and managing oral allergies, it can involve various diagnostic approaches.
- Imaging Studies: For suspected deeper issues like tumors, abscesses (e.g., a peritonsillar abscess), or structural abnormalities beyond what's visible, X-rays, CT scans, or MRI might be ordered. These provide detailed cross-sectional images of the throat and surrounding structures.
- Sleep Study (Polysomnography): If an elongated or swollen uvula is suspected to be causing obstructive sleep apnea, an overnight sleep study will be conducted. This monitors your breathing patterns, heart rate, oxygen levels, and other vital signs while you sleep, providing definitive evidence of sleep-disordered breathing. Understanding the diagnostic and treatment pathways for sleep apnea is crucial for those experiencing related symptoms.
Step 4: Referral to Specialists
Sometimes, the complexity of a uvula pathology requires specialized expertise. Your primary care doctor may refer you to:
- Otolaryngologist (ENT specialist): For detailed assessment, potential biopsy of suspicious lesions, and surgical treatment.
- Allergist/Immunologist: If inflammation is primarily driven by allergic reactions.
- Speech therapist: If uvular abnormalities are affecting speech quality or causing articulation problems.
- Sleep specialist: For comprehensive management of sleep apnea.
Step 5: Discuss Diagnosis and Treatment Options
Once all necessary information is gathered, your doctor will explain their findings. They'll discuss whether the condition is benign, a congenital anomaly, or a pathological concern. Treatment plans are highly individualized and depend entirely on the root cause:
- Infections: Bacterial infections are typically treated with antibiotics; viral infections often require supportive care (rest, fluids, pain relievers).
- Allergies: Management includes antihistamines, corticosteroids, and avoidance strategies for identified allergens.
- Sleep Apnea: For severe cases involving an elongated or swollen uvula, surgical options like uvulectomy (partial or complete removal of the uvula) might be considered.
- Congenital Anomalies: Conditions like a bifid uvula often require no treatment unless they cause functional problems.
- Traumatic Injuries: Supportive care, pain management, and monitoring are usually sufficient.
Throughout this process, open communication with your doctor is vital. Discuss any concerns, side effects from medication, or changes in your symptoms.
Step 6: Follow-Up Monitoring
Regular follow-up is crucial to ensure the condition has resolved, especially after surgery or if you're on long-term medication. This involves re-examination and check-ins to monitor progress. It's important to seek immediate re-evaluation if your symptoms persist, worsen, or if new concerns arise, such as increasing difficulty swallowing or the onset of a fever.
AI Takes the Stage: Revolutionizing Uvula Diagnosis
The diagnostic journey, while thorough, can sometimes be lengthy, requiring multiple appointments and tests. This is where artificial intelligence is beginning to make a transformative impact, promising to make the diagnosis of uvula pathologies faster, more accurate, and potentially more accessible. The integration of Uvula Pathologies & AI Diagnosis marks a significant leap forward in healthcare.
How AI Can Assist: A New Era of Detection
AI's strength lies in its ability to process vast amounts of data, recognize complex patterns, and learn from experience at a scale humans cannot. For uvula diagnostics, this translates into several key applications:
- Enhanced Image Recognition: AI algorithms can be trained on extensive datasets of uvula images—showing normal uvulas, those with uvulitis, lesions, bifid anomalies, or tumors. When a doctor uploads an image from a physical exam or a scope, the AI can quickly analyze it, highlighting suspicious areas, measuring inflammation, or identifying subtle changes that might be missed by the human eye, especially in early stages. This acts as a powerful "second opinion" or an initial screening tool.
- Symptom Pattern Detection: By analyzing patient-reported symptoms, medical history, and risk factors, AI can help connect the dots faster. For instance, if a patient reports persistent snoring, difficulty swallowing, and a dry mouth, an AI system might flag a higher probability of an elongated uvula or sleep apnea, prompting specific diagnostic steps sooner.
- Risk Assessment and Predictive Analytics: AI can leverage population health data to identify individuals at higher risk for certain uvula pathologies based on demographics, lifestyle, and genetic predispositions. This could lead to proactive screenings or lifestyle recommendations.
- Decision Support Systems: For busy clinicians, AI can serve as an intelligent assistant, offering differential diagnoses, suggesting relevant diagnostic tests based on current symptoms, and even outlining potential treatment pathways. This can standardize care and reduce diagnostic errors.
Benefits: Speed, Accuracy, and Accessibility
The advantages of incorporating AI into uvula diagnostics are compelling:
- Faster Diagnosis: AI's rapid analytical capabilities can shorten the time from symptom onset to definitive diagnosis, reducing patient anxiety and allowing for quicker initiation of treatment.
- Increased Accuracy: By identifying subtle features and complex patterns, AI can augment human expertise, leading to more precise diagnoses, especially for rare or early-stage conditions.
- Improved Accessibility: In remote areas or settings with limited specialist access, AI-powered tools could enable primary care providers to conduct more sophisticated initial screenings, guiding referrals more effectively.
- Reduced Burden on Specialists: By streamlining the initial diagnostic process, AI can free up specialists to focus on more complex cases requiring in-depth human intervention.
Current Limitations and Future Outlook
While promising, AI in uvula diagnosis is still evolving. Challenges include ensuring the quality and diversity of training data, addressing potential biases in algorithms, and integrating these tools seamlessly into clinical workflows. Regulatory approvals and ethical considerations around data privacy and diagnostic responsibility also need careful navigation.
However, the future is bright. As AI models become more sophisticated and data sources expand, we can expect even more intuitive and powerful tools. Imagine a future where your doctor uses an AI-powered scope that immediately flags potential issues, or where an AI assistant helps tailor a prevention plan based on your unique risk profile. To dive deeper into how this technology works, you might want to explore the uvula AI generator. It's clear that AI is not here to replace human doctors but to empower them with unparalleled analytical capabilities, ultimately leading to better outcomes for patients grappling with uvula pathologies.
From Diagnosis to Relief: Understanding Treatment Options
Once your uvula pathology is accurately diagnosed, the next step is a tailored treatment plan designed to alleviate symptoms and resolve the underlying issue. The approach can vary significantly, from simple home remedies to medication or even surgical intervention.
Treating the Root Cause
- Infections: If a bacterial infection like strep throat is the culprit behind uvulitis, a course of antibiotics will typically be prescribed. For viral infections, which commonly cause sore throats, antibiotics are ineffective. Instead, treatment focuses on supportive care: rest, staying hydrated, gargling with warm salt water, and over-the-counter pain relievers to manage symptoms.
- Allergies: When allergic reactions trigger uvula swelling, antihistamines can help reduce inflammation. In some cases, corticosteroids might be used for more severe swelling. Identifying and avoiding specific allergens is also a crucial long-term strategy.
- Acid Reflux (GERD): If acid reflux is irritating your uvula, treatment involves medications like antacids or proton pump inhibitors to reduce stomach acid, along with lifestyle changes such as dietary adjustments and elevating the head of your bed.
- Traumatic Injuries: Minor injuries usually heal with supportive care, including pain management and avoiding further irritation. Severe trauma might require more intervention.
Surgical Interventions
For certain conditions, surgery may be the most effective solution:
- Uvulectomy: If an elongated or severely swollen uvula contributes significantly to obstructive sleep apnea or causes chronic gagging and choking, a uvulectomy (the partial or complete removal of the uvula) may be recommended. This procedure aims to clear the airway and reduce irritation.
- Lesion Removal: Benign growths like papillomas or suspicious lesions will often be surgically removed, sometimes followed by a biopsy to confirm their nature.
- Congenital Anomalies: A bifid uvula typically requires no treatment unless it's associated with a submucous cleft palate causing speech or feeding difficulties, in which case corrective surgery might be considered.
Remember, discussing all potential risks, benefits, and alternative treatments with your doctor is essential before making any decisions about surgical options.
Proactive Uvula Care: Preventing Future Issues
While not every uvula abnormality can be prevented, adopting certain habits and practices can significantly reduce your risk of developing many common issues. Proactive care is all about maintaining a healthy throat environment and minimizing exposure to irritants.
Here's how you can protect your uvula:
- Avoid Smoking and Vaping: Tobacco smoke and vaping aerosols are harsh irritants that can inflame the uvula and surrounding tissues, increasing susceptibility to uvulitis and other problems. Quitting is one of the most impactful steps you can take.
- Stay Well-Hydrated: Drinking plenty of water keeps your throat moist and helps your body's immune system function optimally. Dehydration can lead to a dry, irritated throat, making the uvula more vulnerable.
- Manage Acid Reflux (GERD): Stomach acid splashing back into the throat can severely irritate the uvula. If you suffer from GERD, diligently follow your treatment plan and make recommended lifestyle changes to minimize reflux episodes.
- Practice Good Oral Hygiene: Regular brushing, flossing, and mouth rinsing help reduce the bacteria load in your mouth and throat, which can prevent infections that might spread to the uvula.
- Use Humidifiers: In dry environments, especially during winter or in air-conditioned spaces, a humidifier can help maintain moisture in the air, preventing your throat from drying out overnight.
- Promptly Address Upper Respiratory Infections: Don't let colds, flu, or sore throats linger. Early treatment can prevent infections from spreading or worsening, potentially affecting your uvula.
- Limit Alcohol Consumption: Excessive alcohol can act as a diuretic, leading to dehydration, and can also directly irritate throat tissues.
By incorporating these simple yet effective strategies into your routine, you can significantly contribute to the long-term health and well-being of your uvula.
Your Questions Answered: Uvula Health FAQs
You've got questions about that little dangly bit in your throat, and we've got answers. Here are some common queries and misconceptions surrounding uvula health.
Q: Can stress affect my uvula?
A: While stress doesn't directly cause uvula pathologies, it can indirectly impact your throat health. Chronic stress can weaken your immune system, making you more susceptible to infections that might cause uvulitis. It can also exacerbate conditions like acid reflux, which can irritate the uvula.
Q: Is it normal for my uvula to move when I breathe?
A: Yes, it's completely normal for your uvula to move. It's a muscular structure that contracts and relaxes, especially during breathing, speaking, and swallowing. It might appear to "flutter" or swing slightly. Concerns arise when its movement is restricted, or it causes symptoms like gagging.
Q: What's the difference between a sore throat and uvulitis?
A: A sore throat is a general symptom indicating inflammation or irritation anywhere in the throat. Uvulitis is a specific type of inflammation focused only on the uvula. While uvulitis often causes a sore throat, you can have a sore throat without uvulitis (e.g., from a viral infection affecting your whole pharynx).
Q: Can diet impact uvula health?
A: Yes, indirectly. A diet high in acidic foods or drinks can worsen acid reflux, potentially irritating the uvula. Conversely, a healthy, balanced diet supports overall immune function, making you less prone to infections that could affect the uvula. Staying hydrated is also crucial.
Q: Should I worry if I have a bifid uvula?
A: In most cases, a bifid uvula is a benign anatomical variation and causes no problems. It's often discovered by chance. However, in rare instances, it can be associated with a submucous cleft palate, which might lead to speech or feeding difficulties. If you have a bifid uvula and experience related symptoms, it's worth discussing with your doctor.
Q: Can uvula problems cause bad breath?
A: Yes, infections of the uvula or surrounding throat tissues can certainly lead to bad breath (halitosis). The bacteria causing the infection can produce foul-smelling compounds. Resolving the underlying infection typically resolves the bad breath.
Navigating Your Path to Uvula Health with Confidence
Your uvula, though small, is an integral part of your well-being. From ensuring smooth speech and swallowing to playing a role in your body's defenses, its health is paramount. When symptoms arise, whether it's a persistent sore throat, difficulty swallowing, or a visible change, taking action is the smartest move.
We've covered the common uvula pathologies, walked through the comprehensive diagnostic steps your doctor will take, and explored the exciting frontier of how Uvula Pathologies & AI Diagnosis is poised to make detection faster and more accurate than ever before. This blend of traditional medical expertise with advanced technology means you can approach concerns about your uvula with greater confidence.
Remember, knowledge is power. By understanding the signs, knowing when to consult a medical professional, and embracing preventive measures, you're better equipped to maintain your throat health. Don't hesitate to seek medical advice if your symptoms persist or worsen. Your proactive approach ensures that your unsung hero—your uvula—continues to perform its vital roles seamlessly, keeping you comfortable and healthy.